Prostate cancer surgery, a surgical procedure, entails removing the prostate gland and surrounding tissues affected by prostate cancer, a prevalent type of cancer among older males.
This surgery offers potential benefits like eliminating cancerous cells, potentially curing the disease, and alleviating associated symptoms. A significant historical development was the introduction of robotic-assisted laparoscopic prostatectomy, enhancing precision and recovery.
Delving further into prostate cancer surgery, this article explores its types, preparation, recovery process, and potential risks and complications.
Prostate Cancer Surgery
Prostate cancer surgery entails a multitude of essential aspects that shape its significance and impact on patients. These include:
- Prognosis
- Treatment Options
- Recovery Time
- Continence
- Erectile Function
- Cost
- Side Effects
- Mortality Rate
Understanding these aspects is crucial for informed decision-making and navigating the complexities of prostate cancer surgery. Each aspect holds implications for a patient's health, lifestyle, and overall well-being. By delving into these key considerations, patients and their families can gain a comprehensive perspective on prostate cancer surgery and its potential impact.
Prognosis
Prognosis, a crucial aspect of prostate cancer surgery, encompasses the predicted course of the disease and the likelihood of its recurrence after treatment. It involves evaluating diverse factors that influence a patient's outcome and long-term health prospects.
-
Gleason Score
A system that grades prostate cancer cells based on their appearance under a microscope, with higher scores indicating a more aggressive form of cancer and potentially worse prognosis.
-
PSA Level
Prostate-specific antigen (PSA) is a protein produced by the prostate gland, and elevated levels can indicate the presence of prostate cancer. A higher PSA level prior to surgery may suggest a more advanced stage of cancer and affect prognosis.
-
Surgical Margin Status
The presence or absence of cancer cells at the edges of the prostate gland after surgery. Positive surgical margins indicate that the cancer may not have been completely removed, which can impact prognosis and the need for further treatment.
-
Lymph Node Involvement
The spread of cancer to nearby lymph nodes can affect prognosis. The number and location of affected lymph nodes provide valuable information about the extent of the disease and potential outcomes.
These factors collectively contribute to determining the prognosis of prostate cancer surgery, guiding treatment decisions, and providing patients with a realistic understanding of their health trajectory. A thorough assessment of these prognostic indicators allows for personalized treatment plans, appropriate monitoring, and informed decision-making throughout the prostate cancer journey.
Treatment Options
In the realm of prostate cancer surgery, treatment options play a pivotal role in shaping the course of action and determining the effectiveness of the surgical intervention. These options encompass a spectrum of approaches, each tailored to the unique characteristics of the patient and the stage of their disease.
The selection of treatment options hinges upon a comprehensive evaluation of various factors, including the patient's age, overall health, and the extent of cancer spread. The primary goal of prostate cancer surgery is to remove the cancerous prostate gland, and in some cases, nearby lymph nodes, with the utmost precision and minimal impact on surrounding structures. Treatment options may include radical prostatectomy, robotic-assisted laparoscopic prostatectomy, and external beam radiation therapy, among others.
The choice of treatment option significantly influences the outcomes of prostate cancer surgery. For instance, radical prostatectomy, which involves the complete removal of the prostate gland, offers the highest chance of cancer eradication but may come with potential side effects such as incontinence and erectile dysfunction. On the other hand, robotic-assisted laparoscopic prostatectomy employs a minimally invasive approach, reducing the risk of complications while preserving continence and erectile function to a greater extent. Understanding the nuances of each treatment option empowers patients to make informed decisions, in collaboration with their healthcare providers, regarding the most suitable course of action for their specific situation.
Recovery Time
Recovery time, a crucial aspect of prostate cancer surgery, encompasses the period following the procedure when the body heals and regains its normal functions. Understanding the different facets of recovery time is essential for patients undergoing this surgery.
-
Hospital Stay
Typically lasting a few days, the hospital stay provides close monitoring and pain management in the immediate post-operative period.
-
Catheter Removal
A catheter, inserted during surgery to drain urine, is usually removed within a week, allowing patients to regain urinary function.
-
Physical Recovery
Involving restricted activities and wound care, physical recovery can take several weeks, gradually returning patients to their previous activity levels.
-
Functional Recovery
Related to regaining continence and erectile function, functional recovery varies among patients and may require rehabilitation or other therapies.
The recovery time for prostate cancer surgery can vary depending on the type of surgery performed, the patient's age and overall health, and the presence of any complications. Patients should follow their doctor's instructions carefully during the recovery period to ensure a smooth and successful outcome.
Continence
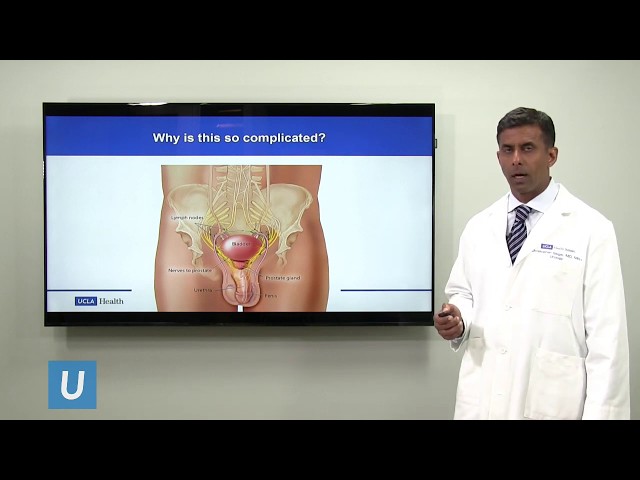
Continence, the ability to control urination and bowel movements, is a crucial aspect of overall well-being. Prostate cancer surgery may impact continence due to its proximity to the urethra and sphincter muscles responsible for urine flow. During surgery, these structures can be affected, leading to varying degrees of incontinence.
The type of surgery performed also influences the risk of incontinence. Radical prostatectomy, which involves removing the entire prostate gland, carries a higher risk of incontinence compared to other less invasive procedures. Additionally, factors such as the patient's age, overall health, and the experience of the surgeon can impact continence outcomes.
Incontinence following prostate cancer surgery can range from mild to severe. Some patients may experience occasional leakage, while others may have difficulty controlling urination completely. Treatment options for incontinence include lifestyle modifications, medications, and surgical procedures. Pelvic floor exercises, which strengthen the muscles supporting the bladder and urethra, can also improve continence.
Managing incontinence after prostate cancer surgery requires a multifaceted approach. Open communication between the patient and healthcare team is essential to determine the best course of action. With proper care and support, most patients can regain or maintain continence following prostate cancer surgery.
Erectile Function
Erectile function, a crucial aspect of male sexual health, can be affected by prostate cancer surgery due to the proximity of the prostate gland to nerves and blood vessels involved in achieving and maintaining an erection. During surgery, these structures can be affected, leading to varying degrees of erectile dysfunction (ED).
The type of surgery performed also influences the risk of ED. Radical prostatectomy, which involves removing the entire prostate gland, carries a higher risk of ED compared to other less invasive procedures. Additionally, factors such as the patient's age, overall health, and the experience of the surgeon can impact erectile function outcomes.
The impact of ED following prostate cancer surgery can be significant, affecting a patient's quality of life and emotional well-being. Treatment options for ED include medications, such as phosphodiesterase type 5 inhibitors (PDE5 inhibitors), and devices, such as vacuum erection devices or penile implants. Pelvic floor exercises, which strengthen the muscles supporting the penis, can also improve erectile function.
Open communication between the patient and healthcare team is essential to determine the best course of action for managing ED after prostate cancer surgery. With proper care and support, many patients can regain or maintain erectile function, preserving an important aspect of their physical and emotional health.
Cost
Within the realm of prostate cancer surgery, the aspect of "Cost" holds significant implications, encompassing a multitude of factors that influence the overall financial burden associated with this medical procedure. This exploration delves into four key facets of "Cost":
-
Surgical Fees
Encompassing the charges for the surgeon's expertise and the surgical team's services during the procedure.
-
Hospitalization
Including the cost of the operating room, anesthesia, and hospital stay, which can vary depending on the length of the surgery and any complications.
-
Pathology and Imaging
Covering the expenses of biopsies, laboratory tests, and imaging studies used for diagnosis and surgical planning.
-
Follow-Up Care
Involving regular check-ups, monitoring, and potential additional treatments or therapies required after surgery.
The overall cost of prostate cancer surgery is influenced by a combination of these factors, as well as the complexity of the surgery, the patient's insurance coverage, and the location of the medical facility. Understanding the financial implications associated with prostate cancer surgery empowers patients to make informed decisions regarding their treatment options and to plan for the potential costs involved.
Side Effects
Regarding "prostate cancer surgery", the aspect of "Side Effects" holds significant relevance. Understanding these potential consequences empowers patients to make informed decisions about their treatment options. This exploration delves into four distinct facets of "Side Effects", providing insights into their implications and real-life examples.
-
Incontinence
After surgery, some patients may experience varying degrees of difficulty controlling urination. This can range from occasional leakage to complete loss of bladder control.
-
Erectile Dysfunction
Prostate cancer surgery may affect nerves and blood vessels responsible for achieving an erection, potentially leading to erectile dysfunction.
-
Pain and Discomfort
Patients may experience pain, discomfort, or numbness in the surgical area, which can typically be managed with medication.
-
Lymphedema
Surgery can sometimes damage lymph nodes, leading to fluid build-up and swelling in the legs or pelvic area.
The severity and duration of these "Side Effects" can vary depending on individual factors, the extent of the surgery, and the patient's overall health. Patients should discuss potential "Side Effects" with their healthcare team before surgery to understand the risks and benefits involved.
Mortality Rate
Mortality rate, a crucial aspect of prostate cancer surgery, encompasses the assessment of patient deaths specifically related to the surgical procedure. This metric holds significant importance in evaluating the safety and effectiveness of surgical interventions.
-
Preoperative Health
A patient's overall health status prior to surgery can influence mortality rate. Factors such as age, comorbidities, and nutritional status play a role in determining surgical risk.
-
Surgical Technique
The expertise and experience of the surgical team, as well as the specific techniques employed, can impact mortality rate. Minimally invasive approaches and robotic-assisted surgery have been associated with lower mortality rates.
-
Postoperative Complications
Complications arising after surgery, such as infection, bleeding, or organ damage, can contribute to increased mortality rate. Prompt management and close monitoring are crucial for minimizing these risks.
-
Long-Term Outcomes
Mortality rate can also be influenced by long-term outcomes, including cancer recurrence and the development of other health conditions. Regular follow-up care and adherence to treatment plans play a vital role in improving overall survival.
Understanding mortality rate helps patients and their families make informed decisions about prostate cancer surgery. By considering individual risk factors, surgical techniques, and potential complications, healthcare professionals can provide personalized guidance and optimize surgical outcomes.
Frequently Asked Questions about Prostate Cancer Surgery
This section provides answers to commonly asked questions about prostate cancer surgery. These questions aim to clarify various aspects of the procedure, helping readers better understand what to expect.
Question 1: What is the purpose of prostate cancer surgery?
Prostate cancer surgery aims to remove the cancerous prostate gland and surrounding tissues to eliminate cancer cells, potentially curing the disease.
Question 2: What are the different types of prostate cancer surgery?
There are several types of prostate cancer surgery, including radical prostatectomy, robotic-assisted laparoscopic prostatectomy, and external beam radiation therapy, each with its unique approach and implications.
Question 3: What are the potential risks and complications of prostate cancer surgery?
Prostate cancer surgery may involve risks such as incontinence, erectile dysfunction, pain, and bleeding. However, advancements in surgical techniques and technologies have minimized these risks.
Question 4: How long does it take to recover from prostate cancer surgery?
Recovery time varies depending on the type of surgery performed and the patient's overall health. Typically, patients can expect to spend a few days in the hospital, followed by several weeks of recovery at home.
Question 5: What is the success rate of prostate cancer surgery?
The success rate of prostate cancer surgery largely depends on the stage of the cancer at the time of diagnosis and the patient's overall health. Early detection and timely intervention can significantly improve the chances of a successful outcome.
Question 6: What are the long-term side effects of prostate cancer surgery?
While most side effects of prostate cancer surgery are temporary, some patients may experience long-term effects such as urinary incontinence or erectile dysfunction. Regular follow-up care and rehabilitation can help manage these side effects.
These FAQs provide a general overview of prostate cancer surgery; however, it is essential to consult with a healthcare professional for personalized advice and guidance.
The next section will delve deeper into the decision-making process involved in choosing the right treatment option for prostate cancer.
Tips for Prostate Cancer Surgery Recovery
Following prostate cancer surgery, a successful recovery is crucial for long-term well-being. Here are some practical tips to aid in your recovery:
Tip 1: Follow Doctor's Instructions
Adhere strictly to your doctor's instructions regarding activity, medications, and wound care to promote proper healing and minimize complications.
Tip 2: Manage Pain Effectively
Take prescribed pain relievers as directed and use non-prescription options like ice packs or heating pads for additional comfort.
Tip 3: Maintain a Balanced Diet
Consume a healthy diet rich in fruits, vegetables, and lean proteins to support your immune system and promote healing.
Tip 4: Stay Hydrated
Drink plenty of fluids, especially water, to prevent dehydration and support urinary function.
Tip 5: Engage in Pelvic Floor Exercises
Practice Kegel exercises to strengthen the pelvic floor muscles, improving urinary and bowel control.
Tip 6: Seek Emotional Support
Connect with family, friends, or support groups to share your experiences and receive emotional encouragement.
Tip 7: Monitor Your Progress
Regularly monitor your recovery and report any unusual symptoms or concerns to your healthcare team promptly.
Tip 8: Be Patient and Positive
Recovery takes time and effort. Stay positive, follow your treatment plan diligently, and celebrate small milestones along the way.
By incorporating these tips into your recovery routine, you can optimize your healing process, improve your quality of life, and maximize the benefits of prostate cancer surgery.
The following section of this article will discuss lifestyle modifications and long-term care considerations to enhance your overall well-being after prostate cancer surgery.
Conclusion
Prostate cancer surgery has emerged as a significant treatment option for localized prostate cancer. The surgical approach, involving the removal of the prostate gland and surrounding tissues, offers the potential for cure. However, the decision-making process is complex, influenced by factors such as cancer stage, patient age, and overall health. Understanding the risks and benefits, recovery process, and potential side effects is crucial for informed decision-making.
One key aspect to consider is the impact on urinary and sexual function. Prostate cancer surgery can lead to varying degrees of incontinence and erectile dysfunction. Open communication with the healthcare team is essential to discuss these potential outcomes and explore strategies for managing them. Psychological and emotional support play a vital role in coping with these changes.