A colorectal cancer screening, also called colon cancer screening, is a series of tests used to find colorectal cancer early.
Colorectal cancer is the third leading cause of cancer-related deaths in the United States. Screening can help find colorectal cancer early, when it is most treatable.
The first colorectal cancer screening test was developed in the 1970s. Since then, there have been many advances in colorectal cancer screening tests. Today, there are several different types of screening tests available, each with its own advantages and disadvantages.
Colorectal Cancer Screening
Colorectal cancer screening is crucial for early detection and prevention. Key aspects to consider include:
- Types of tests
- Frequency
- Preparation
- Accuracy
- Cost
- Risks
- Benefits
- Limitations
- Access
Understanding these aspects helps individuals make informed decisions about screening, optimizing its effectiveness. For instance, knowing the different types of tests available allows for selecting the most appropriate based on individual preferences and health factors. Similarly, being aware of the benefits and limitations guides realistic expectations and supports informed consent.
Types of Tests
Colorectal cancer screening tests vary in their methods, preparation requirements, accuracy, and other factors. Understanding the types of tests available is essential for choosing the most appropriate option.
-
Fecal Occult Blood Test (FOBT)
A simple test that checks for hidden blood in the stool, which may indicate colon cancer or polyps.
-
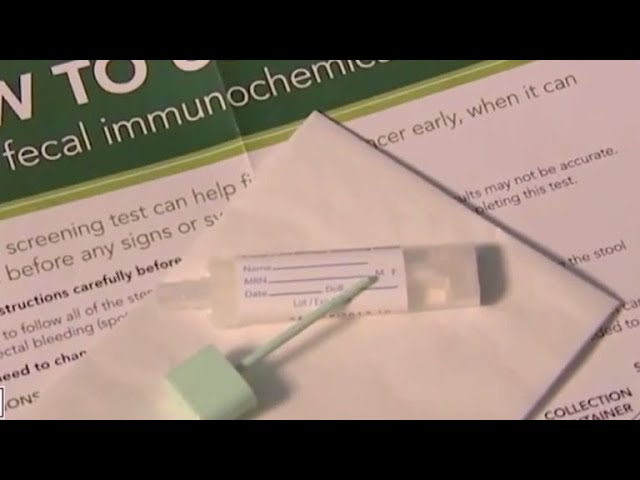
Fecal Immunochemical Test (FIT)
Similar to FOBT, but more sensitive in detecting blood in the stool.
-
Colonoscopy
A procedure where a thin, flexible tube with a camera is inserted into the colon to visualize the lining and remove any polyps.
-
Virtual Colonoscopy (CT Colonography)
A non-invasive imaging test that uses X-rays and computers to create detailed images of the colon.
The choice of test depends on various factors, including age, health history, and individual preferences. Regular screening is crucial for early detection and prevention of colorectal cancer.
Frequency
Frequency of colorectal cancer screening is critical for effective prevention and early detection. Regular screening allows for timely identification and removal of precancerous polyps, reducing the risk of developing colorectal cancer. Studies have consistently demonstrated that individuals who undergo regular screening have a significantly lower incidence of colorectal cancer and improved survival rates compared to those who do not.
The recommended frequency of colorectal cancer screening varies depending on age, risk factors, and personal preferences. However, most guidelines suggest that average-risk individuals should begin screening at age 45 and continue regularly thereafter. For individuals with a family history of colorectal cancer or other risk factors, more frequent screening may be recommended. Regular screening can help detect and remove precancerous polyps before they develop into cancer, thus preventing the onset of the disease.
In summary, frequency is a crucial component of colorectal cancer screening. By adhering to recommended screening intervals, individuals can significantly reduce their risk of developing colorectal cancer and improve their overall health outcomes. Healthcare providers play a vital role in educating patients about the importance of regular screening, addressing any concerns, and ensuring timely access to screening services.
Preparation
Preparation for a colorectal cancer screening is a crucial step that ensures the effectiveness and accuracy of the procedure. It involves a combination of dietary restrictions, lifestyle modifications, and medication adjustments to optimize the visualization of the colon and rectum during the examination.
-
Dietary Restrictions
A few days before the screening, individuals may be required to follow a low-fiber diet to minimize stool residue and enhance the clarity of the colon during the examination.
-
Hydration
Adequate hydration is essential to ensure the effectiveness of bowel preparation solutions. Patients are usually instructed to drink plenty of clear fluids, such as water or broth, to prevent dehydration and facilitate the cleansing process.
-
Medication Adjustments
Certain medications, such as blood thinners or iron supplements, may need to be temporarily adjusted or discontinued before the screening to minimize the risk of bleeding during the procedure.
-
Bowel Preparation
Bowel preparation is a critical part of the preparation process. Patients are typically instructed to consume a specific solution to cleanse the colon and remove stool residue. This solution may be taken orally or administered via enema.
Proper preparation for a colorectal cancer screening enhances the accuracy of the examination, increases the likelihood of detecting polyps or abnormalities, and ensures a safer and more comfortable experience for the patient. By adhering to the preparation guidelines, individuals can contribute to the success of the screening and improve the chances of early detection and prevention of colorectal cancer.
Accuracy
Accuracy is a critical component of colorectal cancer screening. Colorectal cancer screening tests aim to detect precancerous polyps or early-stage cancer, and the accuracy of these tests directly impacts the effectiveness of screening efforts. Highly accurate tests increase the likelihood of detecting abnormal growths, leading to timely interventions and potentially life-saving outcomes.
One of the key measures of accuracy in colorectal cancer screening is sensitivity. A sensitive test has a high probability of correctly identifying individuals with colorectal cancer or precancerous polyps. High sensitivity ensures that a significant number of true positives are detected, reducing the chances of missing cancerous or precancerous lesions.
Specificity is another important aspect of accuracy in colorectal cancer screening. A specific test has a low probability of incorrectly identifying individuals without colorectal cancer as having the disease. High specificity minimizes false positives, reducing unnecessary follow-up procedures and anxiety for patients.
In practical terms, accurate colorectal cancer screening tests enable clinicians to make informed decisions about further diagnostic steps and treatment plans. Accurate test results guide appropriate referrals for colonoscopies or other diagnostic procedures, ensuring timely interventions and improving patient outcomes. Additionally, accurate screening can reduce healthcare costs by avoiding unnecessary and potentially invasive follow-up procedures for individuals without colorectal abnormalities.
Cost
Cost plays a significant role in colorectal cancer screening. The financial implications associated with screening can impact individuals' decisions to participate, potentially affecting early detection and prevention efforts.
Colorectal cancer screening tests vary in their costs, depending on factors such as the type of test, facility, and geographic location. Some screening tests, such as fecal occult blood testing (FOBT) or fecal immunochemical testing (FIT), are relatively low-cost and accessible. However, more advanced procedures like colonoscopy or virtual colonoscopy can be more expensive, requiring specialized equipment and expertise.
The cost of colorectal cancer screening can also vary based on insurance coverage and individual financial circumstances. In some cases, insurance may cover the cost of screening tests, while in other cases, patients may have to pay out-of-pocket expenses. Financial assistance programs may be available for individuals who qualify, helping to reduce the financial burden of screening.
Understanding the cost implications of colorectal cancer screening is crucial for promoting equitable access to these potentially life-saving services. Addressing cost barriers and exploring innovative strategies to reduce financial burden can contribute to increased screening rates, earlier detection, and improved health outcomes for all individuals.
Risks
Understanding the risks associated with colorectal cancer screening is crucial for informed decision-making and optimizing screening strategies.
Colorectal cancer screening procedures, such as colonoscopy or virtual colonoscopy, involve potential risks that should be carefully considered. These risks can be categorized into two main types: procedural risks and risks associated with the preparation process.
Procedural risks may include bleeding, perforation, or infection. While these risks are relatively rare, they can occur during the insertion or withdrawal of the colonoscope or other instruments used during the procedure. The preparation process, which typically involves bowel cleansing, can also pose risks, such as dehydration, electrolyte imbalance, or allergic reactions to the preparation solution.
It's important to note that the benefits of colorectal cancer screening generally outweigh the risks. However, individuals should discuss the potential risks and benefits with their healthcare provider before making a decision about screening. Understanding these risks allows for informed consent and shared decision-making, ensuring that screening is tailored to individual circumstances and preferences.
Benefits
Colorectal cancer screening offers a range of significant benefits, making it a crucial component of preventive healthcare. The primary advantage of screening is the early detection of colorectal cancer and precancerous polyps, increasing the likelihood of successful treatment and improved patient outcomes.
By identifying precancerous polyps during screening, these abnormal growths can be removed before they develop into cancerous tumors. Early detection through screening leads to a higher chance of curative treatment, reducing the risk of colorectal cancer progression and mortality. Additionally, screening can detect colorectal cancer at an early stage, when treatment is most effective, preserving the patient's quality of life and overall health.
Colorectal cancer screening also contributes to cost savings in healthcare. Early detection and treatment of colorectal cancer can prevent the need for more extensive and expensive interventions in the future. Regular screening can reduce the likelihood of advanced-stage cancer, which typically requires more complex and costly treatment modalities. Moreover, screening can help identify individuals at high risk for developing colorectal cancer, allowing for targeted preventive measures and surveillance.
In summary, the benefits of colorectal cancer screening are substantial, including early detection, increased treatment success rates, improved patient outcomes, and potential cost savings. Recognizing the importance of these benefits highlights the critical role of screening as a cornerstone of colorectal cancer prevention and control.
Limitations
Colorectal cancer screening, while effective in reducing colorectal cancer incidence and mortality, has certain limitations that should be acknowledged and addressed. These limitations impact the accuracy, reach, and accessibility of screening, highlighting areas for improvement and optimization.
One significant limitation is the sensitivity and specificity of screening tests. While tests such as colonoscopy and fecal immunochemical testing (FIT) have high sensitivity, they may miss some precancerous lesions or early-stage cancers. False negatives can lead to missed opportunities for early intervention and treatment. Additionally, screening tests may have variable specificity, resulting in false positives that can cause unnecessary anxiety and further testing.
Another limitation relates to accessibility and participation rates. Colorectal cancer screening requires individuals to undergo potentially invasive or unpleasant procedures, which can be a barrier to participation. Access to screening services may also be limited in certain geographic areas or for underserved populations, leading to disparities in screening rates and subsequent health outcomes.
Understanding the limitations of colorectal cancer screening is crucial for optimizing its effectiveness and ensuring equitable access. By addressing these limitations through research, technological advancements, and targeted outreach programs, we can improve the accuracy, reach, and accessibility of screening, ultimately contributing to better colorectal cancer outcomes for all.
Access
Access to colorectal cancer screening is a critical factor that influences its effectiveness and impact on population health. Several facets contribute to the accessibility of screening services, encompassing availability, affordability, and convenience.
-
Geographic Accessibility
Refers to the physical proximity of screening facilities and the ease of transportation to these locations. Individuals living in remote or underserved areas may face challenges in accessing screening services due to distance or lack of transportation options.
-
Financial Accessibility
Relates to the cost of screening and the availability of insurance coverage or financial assistance programs. High costs or lack of insurance can hinder individuals from participating in screening, particularly among low-income or uninsured populations.
-
Cultural and Linguistic Accessibility
Encompasses the availability of culturally sensitive screening materials, interpretation services, and providers who are with diverse cultural backgrounds. Language barriers and cultural beliefs can affect an individual's willingness and ability to undergo screening.
-
Provider Availability
Refers to the number of qualified healthcare providers who offer colorectal cancer screening services. Shortages of providers, particularly in certain geographic areas, can limit access to timely and convenient screening.
Addressing these facets of access is crucial to ensure equitable distribution of colorectal cancer screening services and reduce disparities in health outcomes. By increasing geographic accessibility, providing financial assistance, offering culturally sensitive services, and expanding provider availability, we can improve access to screening and ultimately contribute to better colorectal cancer prevention and control.
Colorectal Cancer Screening FAQs
This section provides answers to frequently asked questions about colorectal cancer screening, addressing common concerns and clarifying key aspects of the procedure.
Question 1: What is the purpose of colorectal cancer screening?
Colorectal cancer screening aims to detect colorectal cancer or precancerous polyps at an early stage, when treatment is most effective and the chances of a cure are higher.
Question 2: Who should get screened for colorectal cancer?
Regular screening is recommended for adults aged 45 or older who are at average risk of colorectal cancer. Individuals with a family history of the disease or other risk factors may need to start screening earlier or more frequently.
Question 3: What are the different types of colorectal cancer screening tests?
Common screening tests include colonoscopy, virtual colonoscopy, fecal immunochemical test (FIT), and guaiac-based fecal occult blood test (gFOBT). Each test has its own advantages and disadvantages, and the best choice depends on individual preferences and health factors.
Question 4: How often should I get screened for colorectal cancer?
The recommended screening interval varies depending on the type of test used and individual risk factors. For average-risk individuals, colonoscopy is typically recommended every 10 years, while FIT or gFOBT may be recommended annually.
Question 5: What are the risks and benefits of colorectal cancer screening?
Screening tests are generally safe, but potential risks include bleeding, discomfort, or complications from the procedure. The benefits of screening include early detection of cancer or precancerous polyps, which can lead to improved treatment outcomes and reduced mortality.
Question 6: What should I do if my screening test results are abnormal?
If a screening test shows an abnormality, further evaluation is necessary to determine the nature of the finding. This may involve additional tests, such as a biopsy or colonoscopy, to confirm a diagnosis and guide appropriate treatment.
These FAQs provide a comprehensive overview of colorectal cancer screening, addressing common questions and emphasizing the importance of regular screening for early detection and prevention. For more detailed information and personalized advice, it is recommended to consult with a healthcare professional.
The next section will delve into the preparation process for colorectal cancer screening, providing step-by-step guidance and tips to ensure a successful and informative experience.
Colorectal Cancer Screening Tips
Preparing for a colorectal cancer screening is essential to ensure the effectiveness and accuracy of the procedure. Here are some practical tips to help you prepare:
Tip 1: Follow the Preparation Instructions Carefully
Read and follow the preparation instructions provided by your healthcare provider. This typically involves dietary restrictions, bowel cleansing, and medication adjustments.
Tip 2: Clear Your Schedule
Plan to have the day of the screening free from other commitments. You may experience some discomfort or fatigue after the procedure.
Tip 3: Arrange for Transportation
If you are undergoing a procedure that requires sedation, arrange for someone to drive you to and from the appointment.
Tip 4: Stay Hydrated
Drink plenty of clear fluids, such as water or broth, before and after the bowel preparation to prevent dehydration.
Tip 5: Get a Good Night's Sleep
Ensure you get a restful night's sleep before the screening to reduce anxiety and promote relaxation.
Tip 6: Inform Your Doctor about Medications
Inform your doctor about all medications you are taking, including prescription drugs, over-the-counter medications, and herbal supplements.
Tip 7: Avoid Alcohol and Smoking
Abstain from alcohol and smoking for at least 24 hours before the screening to minimize any potential interference with the procedure.
Tip 8: Ask Questions and Express Concerns
Do not hesitate to ask your healthcare provider any questions or express any concerns you may have about the screening.
Following these tips can help you prepare effectively for your colorectal cancer screening, ensuring a smooth and successful experience. By being well-prepared, you can maximize the accuracy of the results and contribute to the early detection and prevention of colorectal cancer.
The next section will discuss the importance of regular screening and the benefits it offers in reducing the risk of colorectal cancer.
Conclusion
Colorectal cancer screening plays a vital role in the early detection and prevention of colorectal cancer, a leading cause of cancer-related deaths. Regular screening enables the identification and removal of precancerous polyps, significantly reducing the risk of developing colorectal cancer. The various screening tests available, such as colonoscopy, virtual colonoscopy, and fecal immunochemical testing, offer a range of options tailored to individual preferences and health factors.
Understanding the importance of screening, including its benefits, limitations, and preparation process, empowers individuals to make informed decisions about their health. By addressing barriers to access and promoting equitable distribution of screening services, we can improve population-level colorectal cancer outcomes. Colorectal cancer screening is a crucial component of preventive healthcare, and regular participation is essential for early detection, successful treatment, and improved survival rates.